Introduction:Infections and related complications are a major cause of morbidity and mortality in acute leukemia patients. There is a growing concern for increased antibiotic-resistant organism infections (AROI), including methicillin resistant Staphylococcus aureus pneumonia (MRSA) with the widespread use of antibiotics. Risk factors include older age, prior use of antibiotics, duration of use and type of antibiotics. The role of race, gender, income and insurance status has not been studied. We aimed to study the trends in the prevalence of AROI from 2016 to 2020.
Methods: The National Inpatient Sample (NIS) database was queried to identify adult patients admitted with a principal diagnosis of acute lymphoblastic or myeloid leukemia using the International Classification of Disease (ICD-10) codes. Total leukemia admissions were then analyzed using secondary diagnoses codes for resistance to antimicrobial agents and MRSA pneumonia to assess trends for AROI prevalence and demographic characteristics. Statistics were performed using STATA, and multivariate linear and logistic regression analysis was used to adjust for confounders.
Results:There were a total of 144,385 admissions for acute leukemia in the study period. The leukemia admission rate increased steadily from 2016 to 2020 (p=0.003). A higher proportion of patients belonged to the elderly group (>65 years, 45.2%) compared to middle-aged (45-65 years, 31.9%) and young adults (18-45 years, 22.8%), [p=0.018]. Most of the study population was White (60.9%), followed by Hispanics (15.7%) and African Americans (9.4%). The study population's predominant types of insurance were Medicare (37.5%) and private insurance (38.9%) followed by Medicaid (20.5%).
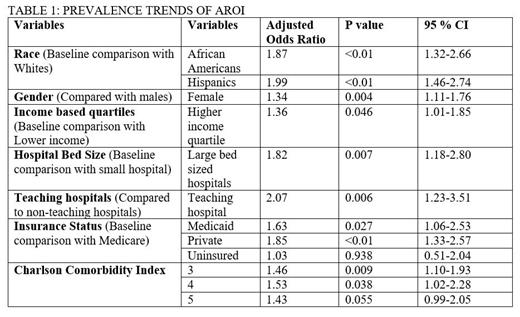
Admissions related to AROI constituted only a small percentage of total leukemia admissions but the proportion of AROI increased from 1.16% in 2016 to 1.90% in 2020 [Adjusted Odds ratio (AOR): 1.12, 95% Confidence Interval (CI)-1.02-1.24; p=0.021]. Woman had a higher prevalence of AROI than men (AOR: 1.39, 95% CI-1.11-1.76; p=0.004). Elderly patients (> 65 years) have nearly similar odds of getting AROI (AOR 1.01) as younger patients (< = 65 years). Compared to Whites, the prevalence trend of AROI is higher in African Americans (AOR: 1.87, 95% CI-1.32-2.66; p<0.01) and Hispanic populations (AOR: 1.99, 95% CI-1.46-2.74; p<0.01).
Higher-income population had increased odds of antibiotic resistance infections than the lower-income population (AOR: 1.36, 95% CI-1.01-1.85; p=0.046). Compared to patients with Medicare, those with Medicaid (AOR: 1.63, 95% CI-1.05-2.52; p=0.027) and Private insurance (AOR: 1.85, 95% CI-1.33-2.57; p=<0.01) had higher AROI, and there was no statistically significant difference with uninsured population. Over the study years, those admitted to larger hospitals (AOR: 1.82; p=0.007) and teaching hospitals (AOR: 2.07; p=0.006) had higher AROI trends than smaller hospitals and non-teaching hospitals respectively. When stratified by Charlson comorbidity index, there was statistically significant trend with increased rates of AROI in patients with lower index points (< = 4) but not in those with higher index points (> 4).
Conclusion:There was a statistically significant rise in the prevalence of AROI across the study years. Racial and economic disparities exist in the prevalence of these resistant infections. Further studies are needed to assess the underlying reasons and steps to address these.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal